Strategy creation must be linked—in real time—to execution plans supported by enterprise performance optimization platforms. We believe this failure to embrace the link between strategy creation and execution is largely due to operating models that do not fully align the organization around planning, performance, and accountability.
A Look at Structure
(Dis)Organization
Typical health system operating models and related viewpoints on organizational management protocols tend to evidence a rigid hierarchical system more akin to “command and control” military organizations than nimble, innovative startups or value-driven private equity firms. We believe this results in a less thoughtful adherence to historical archetypes, planning and performance goals that are not aligned with the requirements of Risk Capability, and a lack of accountability to the more challenging goals required in a sustainable healthcare future state. The standard-issue organization structure consists of:
- A board of directors of a hospital consisting mostly of local and perhaps (depending on institutional size and brand) national business leaders;
- A hospital CEO who reports to the board;
- Chiefs under the CEO who are generally asked to interpret a perhaps vague vision through the lens of their personal responsibilities and associated agendas; various leaders of nurses, HR, IT, finance, and other functions who are often left to do their best operationally with little context for strategic goals or initiatives; clinical managers who worked their way up the ladder who may have little or no formal business or management training; and
- Clinical and support teams who are left to explain a new portal or process to patients and their families with little-known connection to the overall system strategy.
Most of these individuals, and some of their associated teams, were called to healthcare to serve and set about their daily routines doing their absolute best to serve patients and their caregivers. Yet, we have found that there is often little coordination among them and limited connection to the overall organizational strategy. In fact, we often observe fundamental processes working against the achievement of strategic goals.
Consider …
How many times have you seen a strategic plan published after the budget cycle? Or, a budget that is created independently of the endorsed strategy? Such dynamics leave teams pondering how to execute against a strategy without allocated funds.
How often do you see teams working on competing or, if lucky, complementary projects with one team completely unaware of the goals and objectives—or, oftentimes, even the existence—of the other? This dynamic creates inefficiencies, risks the creation of duplicate functions and spend, and often results in an unhealthy, or even toxic, working environment.
(Dis)Economies of Scale
Over the last two decades, health systems have grown tremendously in size and complexity, adding administrative layers and structural intricacies that often separate key players from common, well-aligned goals and make it harder to coordinate and communicate effectively. This growth, whether organic or through mergers and acquisitions, can unexpectedly result in diseconomies of scale.
In many cases, the business thesis driving organic and/or transactional growth demands a fresh look at the organization’s overall operating model, i.e., the fundamental platform that includes governance, leadership, market strategies, core processes, and other critical operating characteristics. Yet rather than rigorously examine their existing operating model in the context of the transforming enterprise, leadership teams simply and habitually insert a carbon copy of corporate management structure that can complicate and confuse planning and obscure decision-making rights and accountabilities. The familiarity of these legacy organizational constructs provides an unwarranted sense of safety, as the resulting misalignments can hinder operational effectiveness and obscure the required linkage to the execution of strategic initiatives. The business strategy and delivery of services have changed, but legacy team structures, leaders, and ways of working live in conflict with the new business. Despite promises of value creation to endorsing, regulating, or investing organizations, e.g., state and local governments, philanthropic stakeholders, or private equity, the resulting operating model is ill-suited for an increasingly outcome-focused, consumer-based industry.
By now, it is well understood that change is a constant. Seemingly less well understood, however, is the required linkage between planning, execution, and accountability that directly impacts an organization’s transformational agility. Traditional constructs simply cannot provide the kind of responsible confidence required to navigate the increasingly dynamic healthcare industry. In the face of these challenges, operating models must evolve to promote agile decision making and drive economies of scale.
A Better Model
From Chaos to Coordination
Modern, nimble, and risk-capable organizations need an optimized operating platform built on an integrated planning and operating framework to aim for successful strategic execution. This platform must provide for quick responses to market dynamics while reinforcing discipline and focus on strategic and operational imperatives. Knowledge of people, change, market, and other industry dynamics is crucial, but possessing this knowledge is not enough. It is imperative to identify and strengthen internal synergies between planning and execution to allow for operations to run smoothly and efficiently, according to a core set of understood, endorsed, and adopted values and beliefs, all focused on unified strategic goals.
Organizations with an optimal operating model anticipate and respond to changes in the market with agility and resolve. Forvis Mazars’ Active Operating Model (AOM) helps focus organizations toward:
- Coordinated planning and execution activities that are guided by mission and strategy
- Enhanced speed, transparency, and accountability in decision making
- Integrated processes and work cycles across various disciplines—resulting in greater system synergy
- Aligned roles, responsibilities, and performance expectations and incentives
- Optimized benefits of scale, innovative care models, and flexible workforce arrangements
Forvis Mazars’ Active Operating Model
The Core:
The Wheel:
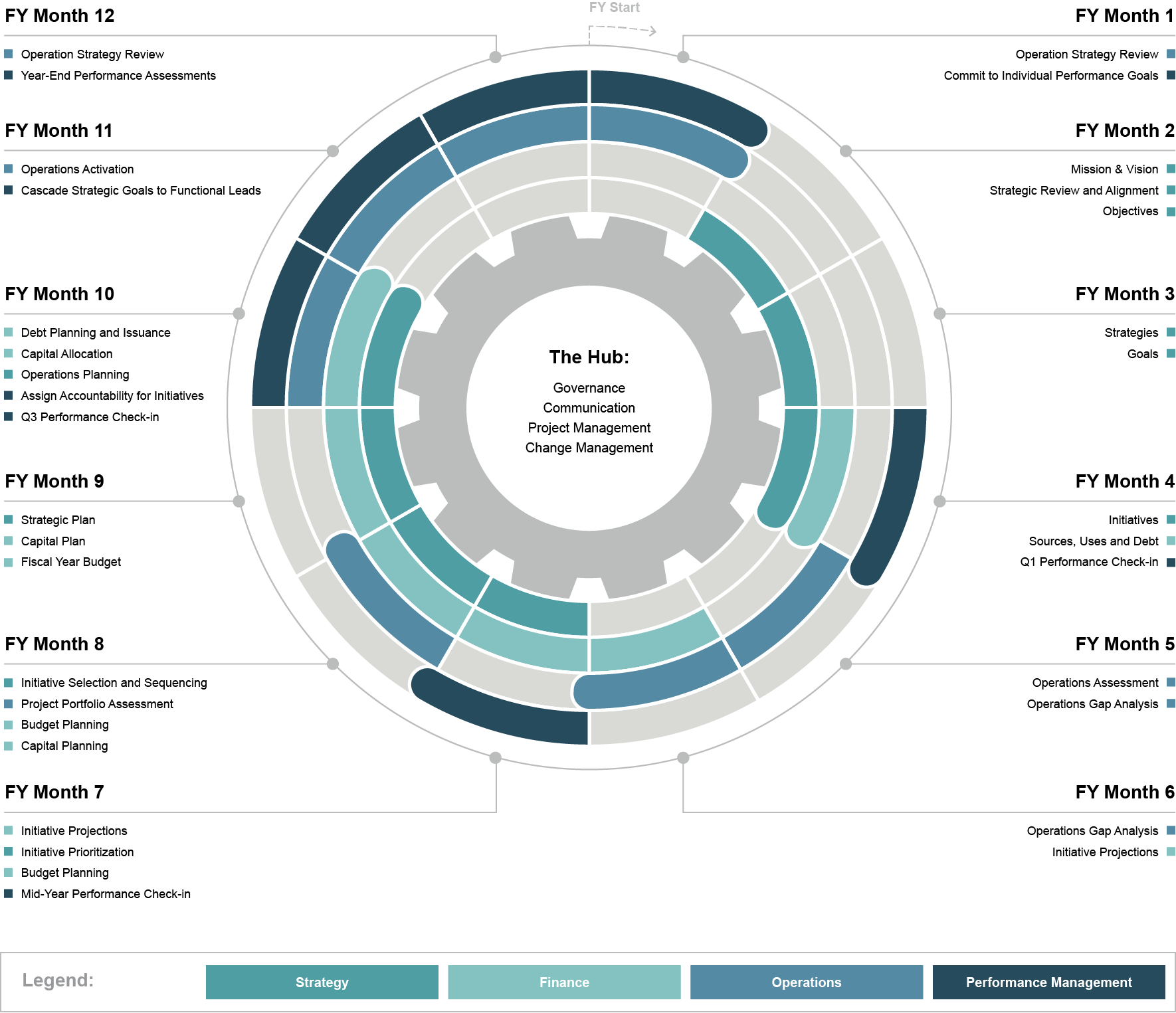
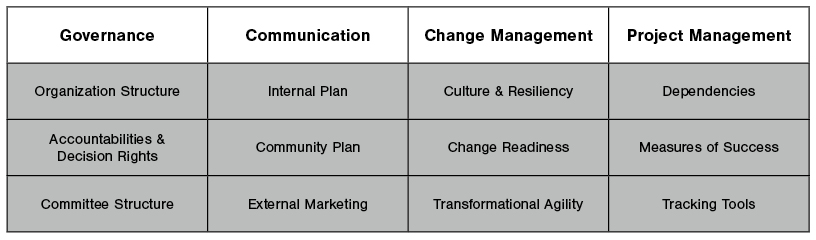
The AOM consists of two main components. First, is the “Core” which provides the discipline, direction, and momentum essential for operational efficiency. It provides the foundational infrastructure that helps maintain all lines of service in the health system ebb and flow in harmony with internal, market, regulatory, and industry changes. These functions—Governance, Communication, Change Management, and Project Management—are critical to nimble, efficient, and effective operations. These organizational capabilities drive the efficiency and effectiveness of the other AOM components that comprise the “Wheel.”
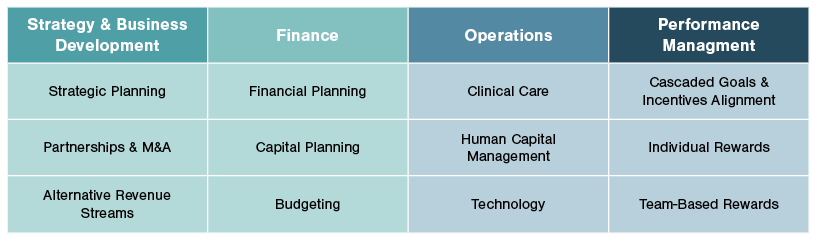
The “Wheel” represents choreographed planning and execution functions—performance management, strategy and business development, finance, clinical and administrative operations that guide the business toward fulfilling its mission. Each function has distinct tasks with defined timing that are essential for a health system to astutely understand market changes, develop response tactics, finance and execute approved strategies, and evaluate and reward staff. Intentionally designed to accommodate each organization’s unique characteristics, the “Core” and “Wheel” create the integrated platform to help drive exceptional execution by fully aligning the organization around planning, performance, and accountability.
The healthcare industry is undergoing seismic shifts that require agile, timely responses. This environment disrupts historical planning and operational norms characterized by five-year plans, static budgeting based on prior years, impulsive prioritization, and hierarchical decision making. However, well-designed strategic plans or decision frameworks are only one part of an effective operating model. A holistic operating model requires a comprehensive and choreographed approach to planning, performance, and accountability.
The Healthcare Practice at Forvis Mazars has long maintained that the changes occurring in our industry demand that health system leadership take a proactive stance with respect to strategies that support risk capability and exceptional execution against those chosen strategies. As we observe health systems routinely struggling to perform against their chosen strategic initiatives, the outmoded nature of historical operating models is evident. We created the AOM to provide a framework that rethinks organizational norms, aims to improve transformational agility, and contributes to the vitality and sustainability of the healthcare industry.
If you have any questions or need assistance, please reach out to a professional at Forvis Mazars.
